Summary of 2023 and Future Reduced Medicare Drug Costs

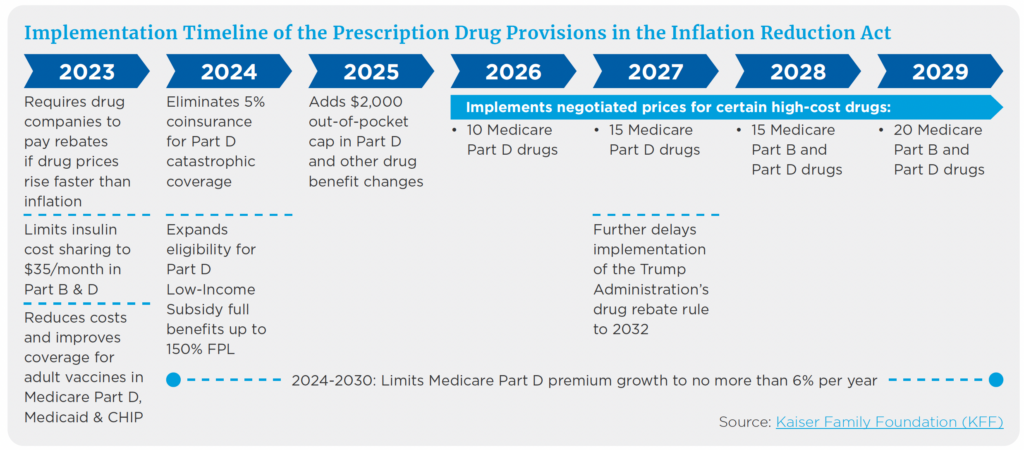
In 2022, President Biden signed legislation that included lowering Medicare prescription drug costs. Some provisions took effect at the start of 2023, while others, like the $2,000 out-of-pocket cap, roll out in 2025. As you plan for health care costs in retirement, consider these current and proposed drug cost changes.
What to Expect From Price Negotiations
Effective this year, the federal government will negotiate prices for certain high-cost drugs, primarily those without a generic or biosimilar equivalent. These drugs include both those covered under Part D of Medicare (retail prescription drugs) and Part B drugs (drugs administered by hospitals).
As noted in the chart, the number of negotiated drugs is limited to 10 Part D in 2026, another 15 Part D in 2027, another 15 Part B and D drugs in 2028, and another 20 Part B and D drugs in 2029 and later years.
How many Medicare beneficiaries will see lower out-of-pocket drug costs in any given year under this provision and the magnitude of savings will depend on which drugs are subject to negotiation, the number of beneficiaries who use those drugs, and the price reductions reached through negotiation.
What to Know About Drug Rebates
Beginning in 2023, drug manufacturers will have to pay rebates to Medicare if prices increase faster than inflation, and 2021 will be used as the base year for determining price changes relative to inflation.
The number of Medicare beneficiaries who may see lower out-of-pocket drug costs in any given year will depend on how many beneficiaries use drugs whose prices increase more slowly than would otherwise occur and the magnitude of price reductions relative to baseline prices.
Caps on Out-of-Pocket Spending
As previously noted, there will be a $2,000 cap on out-of-pocket spending in 2025, which will be especially helpful for beneficiaries who take high-priced drugs to treat health conditions such as cancer or multiple sclerosis.
For example, in 2020, among those Part D enrollees without low-income subsidies, the average annual out-of-pocket spending for the cancer drug Revlimid was $6,200 (used by 33,000 beneficiaries); $5,700 for the cancer drug Imbruvica (used by 21,000 beneficiaries); and $4,100 for the MS drug Avonex (used by 2,000 beneficiaries).1
In addition, starting in 2024, coinsurance, which factors into your out-of-pocket maximum, will be eliminated above the catastrophic threshold. Under current law, the catastrophic threshold is based on the amount beneficiaries pay out-of-pocket plus the value of the manufacturer discount on the price of brand-name drugs in the coverage gap phase.
Limits on Other Increases
The law also limits annual increases in Part D premiums from 2024 to 2030 and makes other changes to the Part D benefit design.
Talk With Your Advisor
As you estimate health care expenses in retirement, Medicare prescription drug costs, along with other costs like premiums, should be included in your cash flow plan.
If you’re already retired, some of these new benefits will help bring overall costs under control. At Mariner, your advisor can meet with you to discuss how to navigate Medicare-related costs and how to figure those into your overall health care costs in retirement.
Sources:
1“How Will the Prescription Drug Provisions Affect Beneficiaries?”
This article is for informational and educational purposes only and should not be interpreted as specific advice. The information contained herein has been obtained from sources believed to be reliable, but we do not warrant the accuracy of the information. Please consult with a qualified professional regarding your personal situation.
Mariner is the marketing name for the financial services businesses of Mariner Wealth Advisors, LLC and its subsidiaries. Investment advisory services are provided through the brands Mariner Wealth, Mariner Independent, Mariner Institutional, Mariner Ultra, and Mariner Workplace, each of which is a business name of the registered investment advisory entities of Mariner. For additional information about each of the registered investment advisory entities of Mariner, including fees and services, please contact Mariner or refer to each entity’s Form ADV Part 2A, which is available on the Investment Adviser Public Disclosure website. Registration of an investment adviser does not imply a certain level of skill or training.
